Abstract
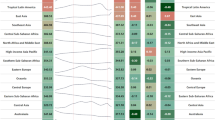
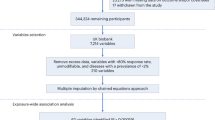
Understanding the lifetime risk of dementia can inform public health planning and improve patient engagement in prevention. Using data from a community-based, prospective cohort study (n = 15,043; 26.9% Black race, 55.1% women and 30.8% with at least one apolipoprotein E4 (APOE ε4) allele), we estimated the lifetime risk of dementia (from age 55 years to 95 years), with mortality treated as a competing event. We applied lifetime risk estimates to US Census projections to evaluate the annual number of incident dementia cases from 2020 to 2060. The lifetime risk of dementia after age 55 years was 42% (95% confidence interval: 41–43). Rates were substantially higher in women, Black adults and APOE ε4 carriers, with lifetime risks ranging from approximately 45% to 60% in these populations. The number of US adults who will develop dementia each year was projected to increase from approximately 514,000 in 2020 to approximately 1 million in 2060. The relative growth in new dementia cases was especially pronounced for Black adults. These results highlight the urgent need for policies that enhance healthy aging, with a focus on health equity.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
ARIC data access procedures are in accordance with participant informed consent and NIH data-sharing policy. Anonymized data from the ARIC study are available at the NHLBI Biologic Specimen and Data Repository Information Coordinating Center and can be accessed through the website (https://biolincc.nhlbi.nih.gov/studies/aric/). Requests for access of ARIC data may also be submitted to the ARIC Publications Committee according to established study procedures, which include submission of a completed ARIC Manuscript Proposal Form (available at https://aric.cscc.unc.edu/aric9/publications/policies_forms_and_guidelines) to the ARIC Publications Committee at aricpub@unc.edu. Review and approval of data access requests typically takes approximately 1 month.
Code availability
The analytic code used for analyses in this study is available from the corresponding author upon reasonable request.
References
Caplan, Z. US older population grew from 2010 to 2020 at fastest rate since 1880 to 1890. United States Census Bureau. https://www.census.gov/library/stories/2023/05/2020-census-united-states-older-population-grew.html (2023).
Rajan, K. B. et al. Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020–2060). Alzheimers Dement. 17, 1966–1975 (2021).
Murphy, S., Kochanek, K., Xu, J. & Arias, E. Mortality in the United States, 2020. NCHS Data Brief, No. 427. National Center for Health Statistics. https://www.cdc.gov/nchs/data/databriefs/db427.pdf (2021).
Nandi, A. et al. Global and regional projections of the economic burden of Alzheimer’s disease and related dementias from 2019 to 2050: a value of statistical life approach. EClinicalMedicine 51, 101580 (2022).
2023 Alzheimer’s disease facts and figures. Alzheimers Dement. 19, 1598–1695 (2023).
Seshadri, S. & Wolf, P. A. Lifetime risk of stroke and dementia: current concepts, and estimates from the Framingham Study. Lancet Neurol. 6, 1106–1114 (2007).
Martin, S. S. et al. 2024 heart disease and stroke statistics: a report of US and global data from the American Heart Association. Circulation 149, e347–e913 (2024).
Chêne, G. et al. Gender and incidence of dementia in the Framingham Heart Study from mid-adult life. Alzheimers Dement. 11, 310–320 (2015).
Beiser, A., Au, R., McNulty, K., White, R. & D’agostino, R. Lifetime risk of dementia and Alzheimer’s disease: the impact of mortality on risk estimates in the Framingham Study. Neurology 49, 1498–1504 (1997).
Licher, S. et al. Lifetime risk of common neurological diseases in the elderly population. J. Neurol. Neurosurg. Psychiatry 90, 148–156 (2019).
Chatfield, M. D., Brayne, C. E. & Matthews, F. E. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. J. Clin. Epidemiol. 58, 13–19 (2005).
Livingston, G. et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396, 413–446 (2020).
Ngandu, T. et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet 385, 2255–2263 (2015).
van Charante, E. P. M. et al. Effectiveness of a 6-year multidomain vascular care intervention to prevent dementia (preDIVA): a cluster-randomised controlled trial. Lancet 388, 797–805 (2016).
Lin, F. R. et al. Hearing intervention versus health education control to reduce cognitive decline in older adults with hearing loss in the USA (ACHIEVE): a multicentre, randomised controlled trial. Lancet 402, 786–797 (2023).
Coley, N., Giulioli, C., Aisen, P. S., Vellas, B. & Andrieu, S. Randomised controlled trials for the prevention of cognitive decline or dementia: a systematic review. Ageing Res. Rev. 82, 101777 (2022).
Williamson, J. D. et al. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA 321, 553–561 (2019).
Lloyd-Jones, D. M. et al. Status of cardiovascular health in US adults and children using the American Heart Association’s new ‘Life’s Essential 8’ metrics: prevalence estimates from the National Health and Nutrition Examination Survey (NHANES), 2013 through 2018. Circulation 146, 822–835 (2022).
Reed, N. S. et al. Prevalence of hearing loss and hearing aid use among US Medicare beneficiaries aged 71 years and older. JAMA Netw. Open 6, e2326320 (2023).
Qian, J. et al. APOE-related risk of mild cognitive impairment and dementia for prevention trials: an analysis of four cohorts. PLoS Med. 14, e1002254 (2017).
Yamazaki, Y., Zhao, N., Caulfield, T. R., Liu, C.-C. & Bu, G. Apolipoprotein E and Alzheimer disease: pathobiology and targeting strategies. Nat. Rev. Neurol. 15, 501–518 (2019).
Fortea, J. et al. APOE4 homozygozity represents a distinct genetic form of Alzheimer’s disease. Nat. Med. 30, 1284–1291 (2024).
Matthews, K. A. et al. Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015–2060) in adults aged ≥65 years. Alzheimers Dement. 15, 17–24 (2019).
Weuve, J. et al. Cognitive aging in black and white Americans: cognition, cognitive decline, and incidence of Alzheimer disease dementia. Epidemiology 29, 151 (2018).
Ferretti, M. T. et al. Sex differences in Alzheimer disease—the gateway to precision medicine. Nat. Rev. Neurol. 14, 457–469 (2018).
Ott, A., Breteler, M. M., Harskamp, F. V., Stijnen, T. & Hofman, A. Incidence and risk of dementia: the Rotterdam Study. Am. J. Epidemiol. 147, 574–580 (1998).
Feigin, V. L. et al. Burden of neurological disorders across the US from 1990–2017: a global burden of disease study. JAMA Neurol. 78, 165–176 (2021).
Vespa, J., Armstrong, D. M. & Medina, L. Demographic Turning Points for the United States: Population Projections for 2020 to 2060 (U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau, 2018).
Wilkinson, T. et al. Identifying dementia cases with routinely collected health data: a systematic review. Alzheimers Dement. 14, 1038–1051 (2018).
Lin, P. J. et al. Dementia diagnosis disparities by race and ethnicity: health services research: cost of care and implications for intervention. Alzheimers Dement. 16, e043183 (2020).
Office of the Assistant Secretary for Planning and Evaluation. US Department of Health and Human Services. National Plan to Address Alzheimer’s Disease. https://aspe.hhs.gov/collaborations-committees-advisory-groups/napa/napa-documents/napa-national-plan (2023).
Wright, J. D. et al. The ARIC (Atherosclerosis Risk in Communities) Study: JACC Focus Seminar 3/8. J. Am. Coll. Cardiol. 77, 2939–2959 (2021).
Knopman, D. S. et al. Mild cognitive impairment and dementia prevalence: the atherosclerosis risk in communities neurocognitive study. Alzheimers Dement. (Amst.) 2, 1–11 (2016).
Knopman, D. S. et al. Patterns of cognitive domain abnormalities enhance discrimination of dementia risk prediction: the ARIC study. Alzheimers Dement. 20, 4559–4571 (2024).
Schneider, A. L. et al. Normative data for 8 neuropsychological tests in older blacks and whites from the Atherosclerosis Risk in Communities (ARIC) study. Alzheimer Dis. Assoc. Disord. 29, 32–44 (2015).
Morris, J. C. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology 43, 2412–2414 (1993).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. ‘Mini-mental state’: a practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198 (1975).
Pfeffer, R. I., Kurosaki, T. T., Harrah, C. Jr, Chance, J. M. & Filos, S. Measurement of functional activities in older adults in the community. J. Gerontol. 37, 323–329 (1982).
Blessed, G., Tomlinson, B. E. & Roth, M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br. J. Psychiatry 114, 797–811 (1968).
McKhann, G. M. et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging–Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 7, 263–269 (2011).
Brandt, J., Spencer, M. & Folstein, M. The telephone interview for cognitive status. Neuropsychiatry Neuropsychol. Behav. Neurol. 1, 111–117 (1988).
Callahan, C. M., Unverzagt, F. W., Hui, S. L., Perkins, A. J. & Hendrie, H. C. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med. Care 40, 771–781 (2002).
Lin, D. Non‐parametric inference for cumulative incidence functions in competing risks studies. Stat. Med. 16, 901–910 (1997).
Stata 18 documentation. https://www.stata-press.com/manuals/documentation-set/
Acknowledgements
This study was supported by National Institutes of Health (NIH)/National Heart, Lung, and Blood Institute (NHLBI) grant K24 HL152440 (to E.S.); NIH/National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant K01 DK138273 (to M.F.); NIH/National Institute on Aging (NIA) grant R01AG054787 (to B.G.W.); the National Institute of Neurological Disorders and Stroke (NINDS) Intramural Research Program (to R.F.G.); and the NIA Intramural Research Program (to K.A.W.). The ARIC study is carried out as a collaborative study supported by NHLBI contracts 75N92022D00001, 75N92022D00002, 75N92022D00003, 75N92022D00004 and 75N92022D00005. The ARIC Neurocognitive Study is supported by U01HL096812, U01HL096814, U01HL096899, U01HL096902 and U01HL096917 from the NIH. The funders had no role in the design and conduct of the study; in collection, management, analysis and interpretation of the data; in preparation, review or approval of the manuscript; and in the decision to submit the manuscript for publication. We thank the staff and participants of the ARIC study for their important contributions. We also thank K. Da Silva and J. Pike for their valuable suggestions and help during revisions.
Author information
Authors and Affiliations
Contributions
M.F. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: M.F. and J.C. Acquisition, analysis or interpretation of data: M.F., J.C., E.S. and J.H. Drafting of the manuscript: M.F. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: J.H. and J.W. Administrative, technical or material support: J.C. and E.S. Supervision: J.C.
Corresponding author
Ethics declarations
Competing interests
D.S.K. has no disclosures relevant to the current work. D.S.K. serves on a Data Safety Monitoring Board for the Dominantly Inherited Alzheimer Network Treatment Unit study. He was an investigator in Alzheimer clinical trials sponsored by Biogen, Eli Lilly Pharmaceuticals and the University of Southern California and is currently an investigator in a trial in frontotemporal degeneration with Alector. He has served as a consultant for Roche, AriBio, Linus Health, Biovie and Alzeca Biosciences but receives no personal compensation. He receives funding from the NIH. The other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Robert Clarke, Bryan James and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary handling editor: Jerome Staal, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fang, M., Hu, J., Weiss, J. et al. Lifetime risk and projected burden of dementia. Nat Med 31, 772–776 (2025). https://doi.org/10.1038/s41591-024-03340-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-024-03340-9