Cost & Value of Medicines


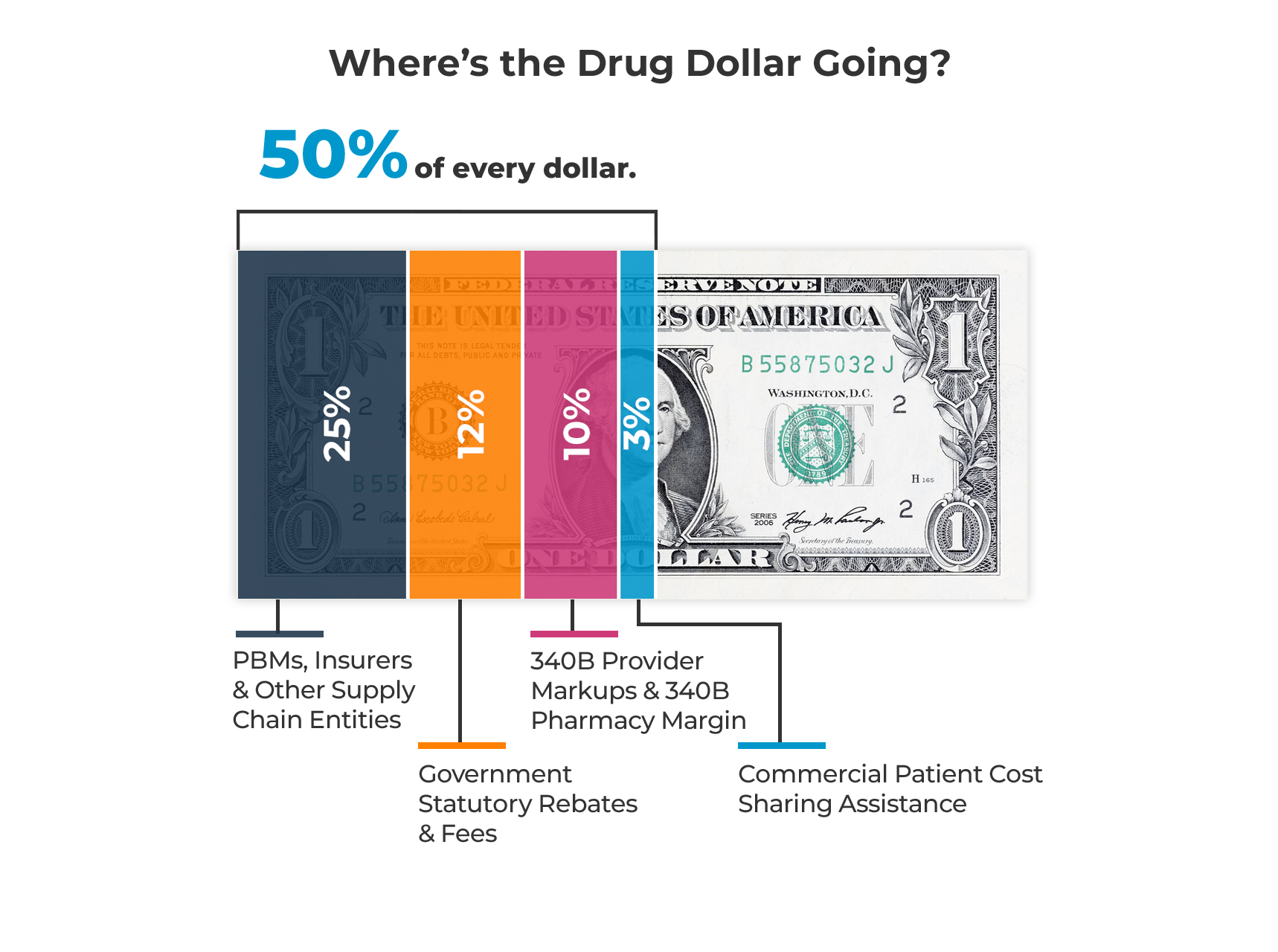
Entities that don’t make medicines get half of what is spent on those medicines.
Half of every dollar spent on brand medicines goes to entities that play no role in the research, development, or manufacturing of those medicines. This highlights a growing problem: spending on medicines is padding the profits of middlemen and subsidizing many parts of the health care system, often at the expense of patients.
Where is the Drug Dollar Going?
It’s going to middlemen like PBMs and insurers who are aggressively consolidating their control over health care; mandatory government fees and rebates; hospitals, clinics and for-profit pharmacies in the 340B markup program; and patient assistance programs designed to help patients in a commercial insurance market that increasingly covers less while charging patients more.
As policymakers continue to look for ways to address rising health care costs and spending on medicines, they must address where half the dollar is going.
12 things to know about the cost and value of medicine.
1. Medical science has never been more promising and despite all the groundbreaking innovation in medicine, spending on medicines remains a small and stable 14% of total health spending.
2. Innovative new medicines not only reduce patients’ need for costly health care services – such as hospital stays and frequent physician visits – but also can generate billions of dollars in savings for the health care system annually. For instance, new brand medicines launched between 2013 and 2017 generated $10 billion in savings across 12 therapeutic areas and lowered net prices. Additionally, breakthroughs like hepatitis C cures are projected to save $43 billion by 2026, and advancements in anti-obesity treatments are transforming care while preventing billions in spending on chronic diseases, the largest driver of U.S. health care costs.
3. Americans have more access to medicine choices than people living anywhere in the world due to our world-leading innovation system. This has resulted in Americans having access to 85% of new medicines compared to less than 40% for Europeans, on average.
4. Medicine costs are the one part of the health care system that decrease over time. For instance, the price of medicines used to prevent cardiovascular disease decreased by 95% over 10 years while the cost of the surgical procedure to treat it increased by 94% over the same period.
5. Competition in the system has led to more treatments available for patients and lower medicine costs, with the net price of brand medicine declining by 3% in 2023 and growing below the rate of inflation over the last five years.
6. More than 90% of all medicines dispensed in the United States are generics, which cost a fraction of the price of the initial brand medicine. The competition from the generic and biosimilar market also leads to savings for the health care system, saving $75 billion from 2013 to 2017 alone and $93.6 billion in projected savings over the next four years.
7. Too many Americans are paying too much for their medicines because actors in the system, like PBMs, insurers, and hospitals are using medicines to subsidize their business. In fact, half of every dollar spent on medicines goes to these actors and others who play no role in the research, development, and manufacturing of them.
8. PBMs and insurers receive billions of dollars in rebates and discounts from pharmaceutical manufacturers annually, which can lower the average price that PBMs and insurers pay by 50% or more, but patients rarely benefit directly from these savings.
9. Accounting for rebates, the net prices PBMs and insurers pay for medicines have grown more slowly than patient out-of-pocket costs since 2016, with the prices patients face growing at a faster rate than the prices insurers face. Insurers are also profiting at patients’ expense by shifting more costs through deductibles and coinsurance, often based on the medicine’s list price—causing some patients to pay more than what insurers or PBMs pay.
10. PBMs make money on medicine’s list price, which experts say leads them to restrict coverage for generics and biosimilars. For instance, between 2014 and 2022, there was a 961% increase in the number of medicines excluded by at least one of the three largest PBMs.
11. Brand manufacturers provided more than $23 billion in patient cost-sharing assistance to commercially insured patients in 2023 alone. Copay accumulator and maximizer programs implemented by PBMs, plans, or other third-party vendors absorbed nearly 45% of patient cost sharing assistance in 2023, more than double the amount attributed to these programs.
12. Hospitals and providers are also driving up costs for patients by using the 340B hospital markup program to subsidize their business. In fact, $65 billion of what is spent on medicines goes to hospitals, clinics, and pharmacies participating in the 340B program. Hospitals markup medicine prices, on average, up to 7x or more.

