Price Setting


Balance the Scales
The United States pays higher drug prices than other countries. Why? Because America is the only country in the world weighed down by 340B hospital markups and PBM middlemen fees driving up costs for patients. At the same time, the United States is forced to subsidize research and development for new treatments and cures, while other countries benefit but don’t pay their fair share.
It’s time to lower drug costs by cracking down on middleman and foreign free riders.
- Fix the 340B hospital markup program. The little-known federal 340B program is a $66 billion program that lets big, tax-exempt hospitals and clinics buy medicines for as little as a penny and then markup the price by thousands of dollars. Hospitals abuse the program to boost their profits at the expense of patients, taxpayers and employers. This program is leading to higher medicine prices in the U.S. Learn more.
- Hold PBMs accountable. In 2023, PBMs took $140 billion in rebates and fees, driving up American medicine costs. These PBM profits may exceed the total cost of drugs overseas. Just three PBMs control nearly 80% of the U.S. market and they dictate what medicines patients can get, what they pay and what hoops they must jump through. Dive deeper.
- Make foreign countries pay their fair share. European countries routinely adopt pricing and reimbursement policies that undervalue medicines, making U.S. patients foot a disproportionate share of the bill for incentivizing the R&D investment for medicines used around the world. These tactics include biased pricing formulas, mandatory discounts, clawbacks and referencing prices paid by lower income countries. Policymakers can use trade negotiations to force countries to pay a minimum percentage of their GDP per capita on new innovative medicines to ensure everyone is paying their fair share.
Government Price Setting has Harmful Consequences for Patients
Government price-setting policies come in a variety of forms, but they all lead to the government inserting itself between patients and providers, threatening access to treatments and chilling research and development of new medicines. In fact, in other countries that have resorted to government price setting, patients have access to fewer new medicines and wait longer to get the medicines they need. Instead of pursuing proposals that could hurt patients and cripple innovation, we need policies that protect access to treatments and make medicines more affordable.
Foreign Reference Pricing
Foreign reference pricing (FRP) is a form of government price setting that effectively outsources drug pricing authority to nations that often undervalue biopharmaceutical innovation and don’t have middlemen like insurers, PBMs and hospitals that distort the system by profiting off treatments.
Why FRP is a bad deal for American patients:
- FRP doesn’t address the real driver of prescription drug costs. The United States is the only country in the world that lets insurers, PBMs, hospitals and others take 50% of every dollar spent on medicines while driving up out-of-pocket costs for patients.
- FRP doesn’t fix unfair practices abroad that put the innovation burden on Americans. Foreign governments routinely undervalue innovative medicines, putting the financial burden of innovation on U.S. patients.
- FRP threatens America’s competitive edge in biopharmaceutical R&D. Imposing price setting would make us less competitive in R&D. There is clear evidence from other countries of the negative impact from government price setting policies. In 1986, biopharmaceutical R&D investment in Europe was 24% higher than in the U.S. After adopting price setting, Europe trails the U.S. by over 40%. Imposing price setting would also make us less competitive with China. Chinese-headquartered companies have the fastest growing clinical trial portfolio in the world, comprising 30% of the world’s clinical trial starts in 2024 up from 1% just a decade earlier.
Solutions should put American patients first. Policymakers should focus on solutions that put American patients first, including reining in middlemen and cracking down on unfair practices abroad, while protecting access to the world’s best doctors, best hospitals and most innovative medicines.

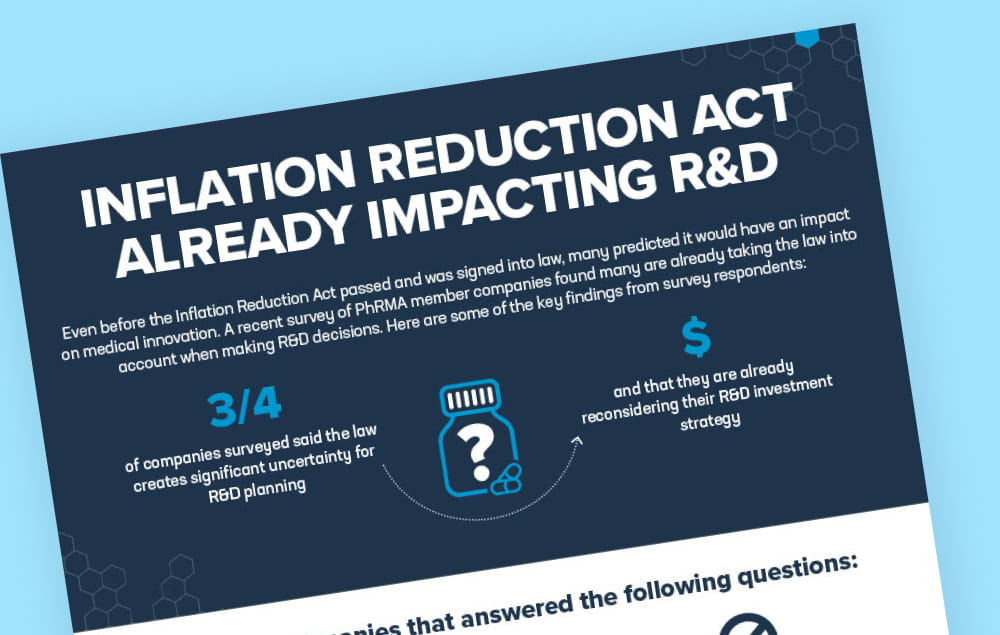
Medicare “Negotiation”
Signed into law in 2022, the Inflation Reduction Act put in place policies that mandate government-set prices for medicines covered by Medicare. These polices are expected to have a negative impact on access to medicines covered by Medicare Part B and Part D, in addition to discouraging continued drug development. The law introduced a ‘pill penalty’ in which the price setting process starts seven years after small molecule medicines (e.g., tablets, capsules and pills) are initially approved by the U.S. Food and Drug Administration (FDA) compared to 11 years after initial FDA approval for large molecule medicines (e.g., biologics that are injected or infused). This system ignores the nature of the research and development (R&D) process, discouraging continued R&D after a medicine is FDA approved and deeming some types of medicines as not worth the real-life impact they can have on patients. This process also ignores how therapeutic value increases over time as medicines are approved for new uses, such as in new patient populations, new diseases or new formulations.

Prescription Drug Boards
Prescription drug boards give bureaucrats the power to arbitrarily set medicine prices in a given state. As a result, decisions about medicines would be a part of a political process that changes with elections and the whims of politicians.
Under this policy, the state would evaluate whether certain medicines and treatments are “worth” paying for, meaning the state’s bureaucracy could come between patients and the treatments their doctors prescribe. This spells disaster for patients as they could face barriers to obtaining lifesaving medications.
Instead of pushing for government price-setting policies like prescription drug boards that assign bureaucrats the power to arbitrarily set medication prices, state leaders can choose to fix a broken health care insurance system without risking patient access, innovation and jobs.
Patients need help affording their medicines at the pharmacy counter, which is why we have consistently supported numerous policies that will directly address this need. Unfortunately, there’s no evidence the prescription board will solve these problems.
Government price setting threatens families’ access to the medicine they need

Ensuring A Better Future For Her Child: Emily H
Caring for a child with a serious illness isn’t easy. "It took us a long time to get answers for him—9 years. And it took going across the country to a specialty clinic." Now Emily is raising her voice to ensure that her son and kids across the country have access to the medicines and new innovation they need.

Patients Like Sue Worry Congress is Compromising Access to Medicines by Meddling with Medicare
Sue is a patient with Type 1 diabetes who depends on Medicare to get her medicines. It’s not always easy. Now some in Congress want to make it harder for patients like Sue to access her medicines. There’s a better way to fix health care for patients.